Reviewed by Brian St. Pierre, MS, RD and Helen Kollias, PhD
It’s like my thoughts were under a pile of garbage.
On a Friday night, as my husband and I tried to figure out where to eat, a typical conversation would go like this:
Me: Do you want to go to that restaurant?
Him: What restaurant?
Me: I can’t think of the name. We’ve eaten there before. It’s that place with the peanut shells on the floor? It’s next to… You know… It’s on that road where we used to take the dog to the vet. Do you know the one I’m talking about??
It was as if certain details got lost in a pile of sludge in the deep recesses of my brain. Then, hours later, the details would escape, and I’d shout into an empty room…
“Texas Roadhouse!”
Sludginess with proper nouns is typical for people who are middle-aged and beyond.
However, what seemed to be happening to me, increasingly in my late 40s and early 50s, felt far from typical.
Not only could I never seem to spit out the names of various restaurants or people or books or movies or so many other things, but my brain was also pooping out during the workday.
I’d sit in front of my computer screen, stare at a document, and will myself to do something constructive with my fingertips. Everything seemed hazy, like those first few moments in the morning when you’re awake enough to turn off the alarm but too sleepy to do basic math.
I had my good moments, usually in the morning, when I attempted to pack eight hours of writing into the two or three hours I possessed mental clarity.
On my worst days, however, I awoke with a haze I never managed to shake. Work was a non-starter. Nor did I have enough bandwidth to read, or do much of anything, really.
I sought medical advice.
Three healthcare professionals recommended antidepressants. I tried one, and felt even worse. I tried another. I tried yet another at a higher dose. Still, I felt like a zombie. Another professional gave me a sleeping pill. It left me feeling even more drugged.
Someone tested my thyroid. There was nothing wrong with it. Nor was I anemic. I tried supplements, mushroom coffee, and just about any product with the word “think” somewhere on its label.
Finally, after nearly two years of seeing a revolving door of doctors, I made an appointment with a gynecologist for my yearly exam. I mentioned vaginal dryness. That information triggered her to ask a string of questions that had nothing to do with my undercarriage. How was my sleep? Mood? Energy levels? Was I experiencing hot flashes? How about brain fog?
“Funny you should mention brain fog,” I said in my usual hazy monotone. “I feel like I’m barely alive.”
By the end of the visit, I understood that I’d likely never had depression.
What I “had” was menopause.
My gynecologist sent me home with prescriptions for estradiol and progesterone.
Within days, it was as if someone had flipped a switch.
I could think again. I could type words again. I could follow conversations. I could work past noon.
And, for the first time in years, I could sleep more than two hours without waking.
Now, menopause isn’t a medical condition.
Nor is it a disease.
Instead, like puberty, it’s a life stage—a transitional moment to be precise.
Once you’ve gone 12 consecutive months without a period, you’ve reached menopause. And from that moment onwards, you’re officially “postmenopausal.”
As women approach this transitional moment, hormone levels fluctuate and fall, triggering dozens of symptoms. Weight gain and reduced sex drive get a lot of attention.
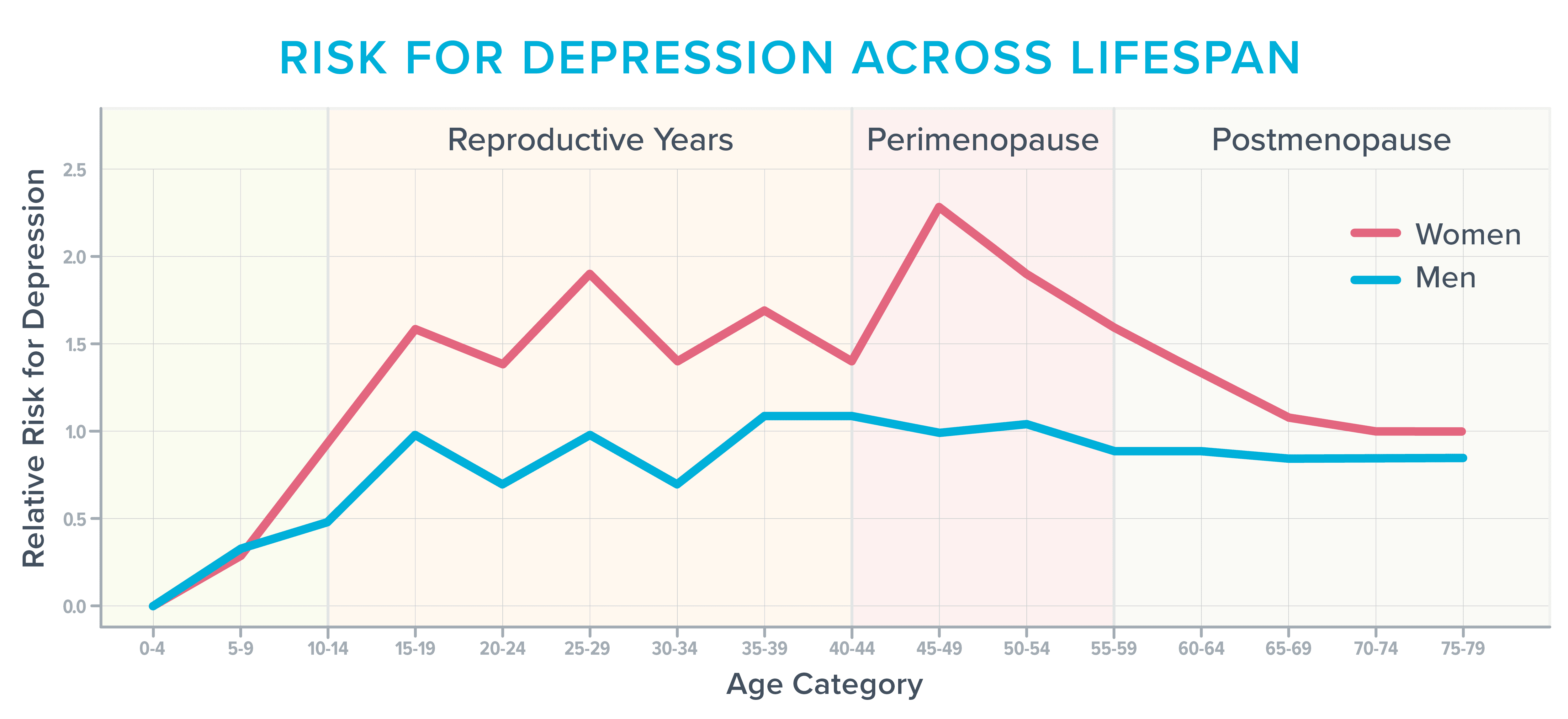
However, during and after menopause, roughly 40 percent of women report increased irritability, mood swings, anxiety, fatigue, and trouble concentrating, according to the American College of Obstetricians and Gynecologists.1 2 As the following image shows, it’s also one of the most vulnerable times in a woman’s life to develop depression,3 particularly if they’ve struggled in the past with it before.
Before starting hormones, I often found myself sobbing for no reason. Other times, the world’s stimuli felt too… stimulating.
Normal everyday sounds—like the buzz of traffic or people at the mall—literally hurt. I was jumpy and irritable and felt anxious about situations that had never bothered me in the past, such as driving over bridges or through construction.
It’s not completely clear what drives these cognitive and emotional symptoms.
Fluctuating hormone levels likely play a role, as do typical age-related changes in the brain.
In addition, during this stage of life, women often deal with several issues that siphon cognitive capacity faster than a thirsty vampire drains a carotid.
During their 40s and 50s, for example, many women have reached the peak of their careers, with responsibilities that follow them home and keep them up at night.
Seeking help for cognitive discontent
For women experiencing cognitive discontent due to hot flashes and night sweats, it’s important to advocate for yourself and seek out healthcare professionals who are knowledgeable about menopause and its symptoms.
Here are some steps you can take:
- Find a healthcare provider who is well-versed in menopause and willing to discuss treatment options with you.
- Be honest and open about your symptoms, including hot flashes, night sweats, and any cognitive changes you may be experiencing.
- Consider keeping a symptom journal to track the frequency and severity of your hot flashes and night sweats, as well as any cognitive symptoms you notice.
- Ask about treatment options, including hormone therapy, lifestyle changes, and other interventions that may help alleviate your symptoms.
- Don’t be afraid to seek a second opinion if you feel your concerns are not being taken seriously or if you are not satisfied with the treatment options presented to you.
Remember, cognitive discontent is a real and valid concern for many menopausal women. By speaking up and seeking help, you can take steps to improve your cognitive health and overall well-being during this transitional time in your life.
Don’t let hot flashes and night sweats go untreated—your brain will thank you for it.
So, consider taking a morning walk outside or sitting by a window with your morning coffee. And if you’re usually indoors during the day, maybe it’s time to think about a light therapy box or lamp.
Strategy #4: Practice stress management techniques.
Stress can exacerbate menopausal symptoms, so it’s important to find ways to manage it. Techniques such as deep breathing, meditation, yoga, tai chi, progressive muscle relaxation, or even just taking a few minutes to sit quietly and focus on your breath can help reduce stress levels.
Strategy #5: Prioritize sleep.
Getting enough quality sleep is crucial for overall health and well-being, especially during menopause. If you’re struggling with sleep disturbances, consider creating a bedtime routine, optimizing your sleep environment, and avoiding caffeine and electronics before bed.
Strategy #6: Stay physically active.
Regular physical activity not only helps with weight management and bone health but can also improve mood and reduce the severity of menopausal symptoms. Aim for at least 150 minutes of moderate-intensity exercise per week, such as brisk walking, swimming, or cycling.
Strategy #7: Connect with others.
Building and maintaining strong social connections can help reduce feelings of isolation and improve mental and emotional well-being. Make an effort to reach out to friends and family, join a club or group, or volunteer in your community.
Strategy #8: Find purpose and meaning.
Having a sense of purpose and meaning in life can help you navigate the challenges of menopause with resilience and positivity. Consider volunteering, pursuing a hobby or passion, or setting new goals for yourself.
Strategy #9: Seek professional help if needed.
If you’re struggling to cope with the physical or emotional symptoms of menopause, don’t hesitate to seek help from a mental health professional. Therapy or counseling can provide you with the tools and support you need to navigate this transitional phase of life.
Remember, menopause is a natural and normal part of the aging process, and while it may come with its challenges, it can also be a time of growth, self-discovery, and empowerment. By taking care of your physical, mental, and emotional health during this time, you can emerge stronger and more resilient than ever.
So, don’t let fear of litigation prevent you from seeking the care and support you need during menopause. Educate yourself, advocate for your health, and prioritize self-care. Your well-being is worth it.
When people spent time outdoors in the mornings, they fell asleep more quickly, slept longer, and experienced fewer awakenings the following evening. Sunlight may also improve mood and concentration.
One strategy to improve sleep and overall well-being is to go easier at the gym. Long, intense exercise sessions can be draining and may lead to injuries or increased irritability. Instead, consider incorporating short bursts of exercise into your day to help you feel more alert.
Another helpful strategy is to investigate Cognitive Behavior Therapy for Insomnia (CBT-I). This therapy can help you develop skills and mental reframes that encourage sound sleep.
It’s also important to get real about stress and prioritize rest and recovery. By analyzing your current responsibilities and making necessary changes, you can reduce stress and improve your overall well-being.
Experimenting with cooling technology, taking frequent breaks, and following a diet that promotes healthy circulation can also contribute to better sleep and cognitive function.
While navigating menopause and the challenges it may bring, it’s important to see this stage of life as an opportunity to re-evaluate priorities and focus on what truly matters. By making small changes and taking care of yourself, you can navigate this stage with grace and resilience.
As I navigated through the challenges of perimenopause, I found myself overwhelmed with the changes in my body and mind. Mood swings, hot flashes, and fatigue became a regular part of my daily life. It was a struggle to balance work, family, and personal time while dealing with these symptoms.
One of the biggest changes I made was to prioritize self-care. I started exercising regularly, eating a healthier diet, and getting enough sleep. These simple changes made a significant impact on my overall well-being and helped me manage the symptoms of perimenopause more effectively.
However, I also realized that simplifying my life was essential. Maybe the recipes I chose could be simplified, too. Finally, maybe saying “no” a lot more often and without regret would allow me to continue to say yes to the things that mattered most. Things like visiting my aging parents, picking up the phone whenever my kid called from college, or meeting a friend for a meandering walk around town.
Thanks to the hormones and life tweaks, I now have energy again. I’m also clear-headed most of the time. However, I still tend to end my workday around 3 p.m. Why? Because I can, and I want to.
Perimenopause is a challenging time in a woman’s life, but with the right strategies and support, it is possible to navigate through it successfully. By prioritizing self-care, simplifying life, and learning to say no, women can manage the symptoms of perimenopause and emerge stronger and more resilient.
The Impact of Lifestyle Factors on Cognitive Performance and Mental Health
In today’s fast-paced world, our cognitive performance and mental health are constantly being challenged by various lifestyle factors. From sleep deprivation to dietary habits, our daily choices play a significant role in shaping our brain function and overall well-being. Recent research has shed light on the profound effects of different lifestyle factors on cognitive performance and mental health.
Single Dose Creatine Improves Cognitive Performance
A study published in Sci Rep revealed that a single dose of creatine can improve cognitive performance and induce changes in cerebral high-energy phosphates during sleep deprivation. This finding suggests that creatine supplementation may have potential benefits for individuals facing cognitive challenges due to lack of sleep.
Sunlight Exposure and Sleep Patterns
Another study published in the Journal of Health Psychology explored the relationship between sunlight exposure and next-night sleep among U.S. adults. The findings indicated that sunlight exposure could predict sleep patterns, highlighting the importance of natural light in regulating our circadian rhythms.
Day and Night Light Exposure and Psychiatric Disorders
Research published in Nature Mental Health demonstrated that day and night light exposure are associated with psychiatric disorders. The study, which involved over 85,000 participants, emphasized the impact of light exposure on mental health outcomes, suggesting a potential link between environmental factors and psychiatric conditions.
Age-Associated Differences in Exercise Recovery
A study published in Cells investigated age-associated differences in recovery from exercise-induced muscle damage. The research highlighted the importance of understanding how age influences the body’s ability to recover from physical exertion, providing valuable insights for tailored exercise interventions.
Mediterranean Diet and Neurodegenerative Diseases
Research published in Neurology explored the association of Mediterranean and DASH diets with Alzheimer’s disease pathology. The study suggested that dietary interventions could play a role in delaying the progression of neurodegenerative diseases, offering new possibilities for managing cognitive decline.
Impact of Dietary Nitrate on Cognitive Function
A study published in Physiology and Behavior examined the effects of dietary nitrate on cerebral blood flow parameters and cognitive performance in humans. The findings indicated that dietary nitrate could modulate brain function and cognitive abilities, highlighting the potential benefits of nitrate-rich foods for cognitive health.
Benefits of the Mediterranean Diet on Mental Health
A literature review published in Clinical Practice and Epidemiology in Mental Health highlighted the benefits of the Mediterranean diet on both physical and mental health. The review emphasized the positive impact of dietary habits on cognitive function and mental well-being, underscoring the importance of a balanced diet for overall health.
Nitrate and Breakfast on Cognitive Function
Another study published in Npj Science Food investigated the effects of nitrate and breakfast on prefrontal cognitive and haemodynamic response functions. The research highlighted the potential cognitive benefits of nitrate-rich foods, suggesting a link between dietary choices and brain function.
Overall, these studies underscore the intricate relationship between lifestyle factors and cognitive performance, emphasizing the importance of healthy habits for optimal brain function and mental well-being.
the title: “The Benefits of Mindful Meditation for Mental Health”
In today’s fast-paced world, it’s easy to become overwhelmed and stressed out. With the constant barrage of information, responsibilities, and distractions, it’s no wonder that mental health issues are on the rise. However, one simple practice that can help combat these challenges is mindful meditation.
Mindful meditation is a practice that involves focusing on the present moment and being aware of your thoughts, feelings, and surroundings without judgment. By cultivating this sense of mindfulness, individuals can reduce stress, anxiety, and depression while improving their overall mental well-being.
One of the key benefits of mindful meditation is its ability to reduce stress levels. When we are constantly bombarded with stimuli and demands, our bodies go into a state of fight or flight, releasing stress hormones that can have a negative impact on our health. By practicing mindful meditation, individuals can activate the body’s relaxation response, leading to a decrease in stress and an increase in feelings of calm and relaxation.
Additionally, mindful meditation can help individuals manage anxiety and depression. By developing a greater sense of awareness and acceptance of their thoughts and emotions, individuals can learn to navigate challenging feelings with more ease and compassion. This can lead to a reduction in symptoms of anxiety and depression, as well as an overall improvement in mood and outlook on life.
Furthermore, mindful meditation has been shown to improve cognitive function and focus. By training the mind to be more present and attentive, individuals can enhance their ability to concentrate, make decisions, and problem-solve. This can lead to increased productivity, creativity, and overall mental clarity.
In conclusion, mindful meditation is a powerful tool for improving mental health and well-being. By incorporating this practice into your daily routine, you can experience decreased stress, anxiety, and depression, as well as increased focus, clarity, and overall happiness. So why not give it a try and see the positive impact it can have on your life?